A student learns what information about acute pancreatitis – Embarking on a journey to unravel the complexities of acute pancreatitis, this comprehensive guide unveils the pathophysiology, clinical manifestations, management strategies, and preventive measures associated with this enigmatic condition. With a focus on equipping students with a profound understanding of the subject matter, this discourse delves into the intricate mechanisms underlying acute pancreatitis, its clinical presentation, diagnostic modalities, therapeutic interventions, and lifestyle modifications aimed at mitigating its occurrence.
Acute pancreatitis, a sudden inflammation of the pancreas, poses a significant health concern, affecting individuals worldwide. Understanding its multifaceted nature is crucial for students aspiring to excel in the medical field. This guide serves as an invaluable resource, providing a comprehensive overview of acute pancreatitis, empowering students with the knowledge and insights necessary to effectively manage this condition in clinical practice.
Pathophysiology of Acute Pancreatitis
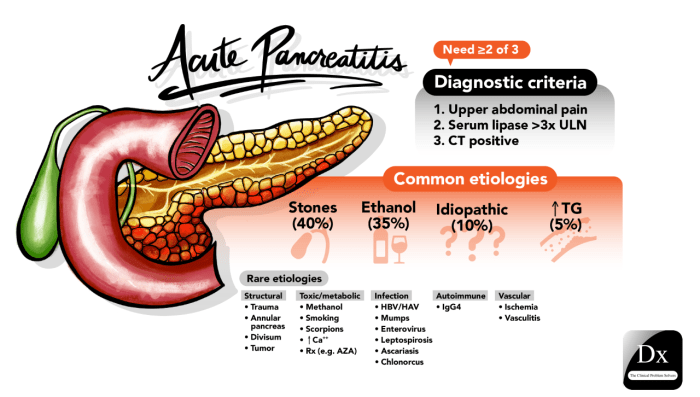
Acute pancreatitis is an inflammatory condition of the pancreas that can range in severity from mild to life-threatening. The inflammatory process involves the activation of pancreatic enzymes, which can lead to autodigestion of the pancreas and surrounding tissues.
Role of Enzymes in the Development of Acute Pancreatitis
The pancreas produces a variety of enzymes that are involved in the digestion of food. In acute pancreatitis, these enzymes become activated prematurely within the pancreas, leading to the destruction of pancreatic tissue and the release of inflammatory mediators.
Potential Complications Associated with Acute Pancreatitis
- Pancreatic necrosis
- Infected pancreatic necrosis
- Pseudocyst formation
- Systemic inflammatory response syndrome (SIRS)
- Multiple organ dysfunction syndrome (MODS)
Clinical Manifestations of Acute Pancreatitis
The most common symptoms of acute pancreatitis include:
- Abdominal pain
- Nausea
- Vomiting
On physical examination, patients may have:
- Tenderness in the upper abdomen
- Epigastric pulsation
- Jaundice
Laboratory and imaging tests used to diagnose acute pancreatitis include:
- Serum amylase and lipase levels
- Abdominal ultrasound
- Computed tomography (CT) scan
Management of Acute Pancreatitis
Conservative Management
The principles of conservative management for acute pancreatitis include:
- Pain control
- Fluid resuscitation
- Nutritional support
Surgical Intervention
Surgical intervention is indicated in patients with:
- Severe necrotizing pancreatitis
- Infected pancreatic necrosis
- Biliary or duodenal obstruction
Potential Complications Associated with the Management of Acute Pancreatitis, A student learns what information about acute pancreatitis
- Infection
- Bleeding
- Pancreatic fistula
- Death
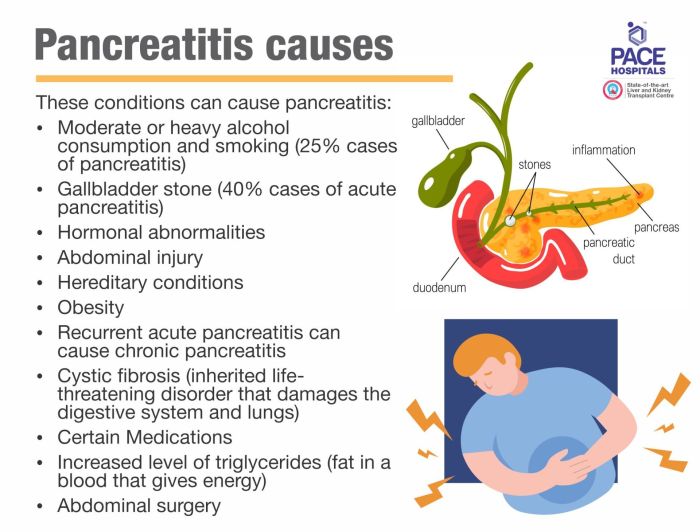
Prevention of Acute Pancreatitis
Modifiable Risk Factors
Modifiable risk factors for acute pancreatitis include:
- Alcohol consumption
- Gallstones
- Hypertriglyceridemia
- Obesity
Lifestyle Modifications
Lifestyle modifications that may help prevent acute pancreatitis include:
- Limiting alcohol intake
- Maintaining a healthy weight
- Eating a healthy diet
- Exercising regularly
Prophylactic Measures
Prophylactic measures that may be considered in high-risk individuals include:
- Endoscopic retrograde cholangiopancreatography (ERCP)
- Cholecystectomy
General Inquiries: A Student Learns What Information About Acute Pancreatitis
What are the common symptoms of acute pancreatitis?
The hallmark symptom of acute pancreatitis is severe abdominal pain, often radiating to the back. Other common symptoms include nausea, vomiting, fever, and abdominal tenderness.
What are the risk factors for developing acute pancreatitis?
Excessive alcohol consumption, gallstones, and certain medications are well-established risk factors for acute pancreatitis. Other factors, such as hypertriglyceridemia and autoimmune disorders, may also contribute to its development.
How is acute pancreatitis diagnosed?
Diagnosis of acute pancreatitis typically involves a combination of clinical examination, laboratory tests (e.g., elevated serum amylase and lipase levels), and imaging studies (e.g., abdominal ultrasound or CT scan).