The newborn with jaundice HESI case study presents a comprehensive overview of the physiological process, causes, symptoms, assessment, diagnosis, treatment, nursing care, and differential diagnosis of neonatal jaundice. This in-depth analysis provides a valuable learning opportunity for nursing students and healthcare professionals.
Jaundice, a common condition in newborns, occurs when bilirubin levels in the blood become elevated, causing a yellowing of the skin and mucous membranes. Understanding the underlying causes, risk factors, and appropriate management strategies is crucial for ensuring optimal patient outcomes.
Jaundice in Newborns
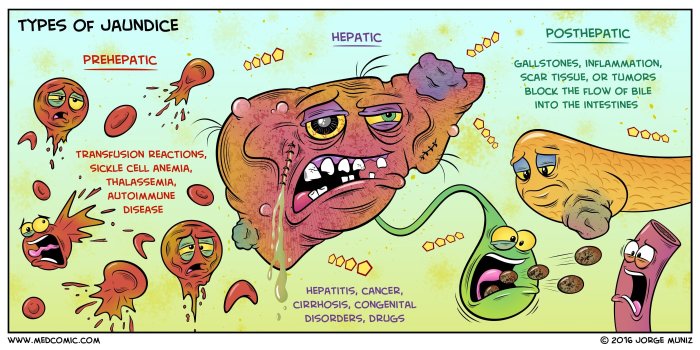
Jaundice is a common condition in newborns, characterized by a yellow discoloration of the skin and mucous membranes due to elevated bilirubin levels. It occurs when the liver, which is responsible for metabolizing and excreting bilirubin, is unable to process the excess bilirubin produced by the breakdown of red blood cells.
Causes and Risk Factors
Physiological jaundice is the most common type of jaundice in newborns, typically appearing within 2-3 days of birth and resolving within 1-2 weeks. It is caused by the increased production and decreased clearance of bilirubin, which is normal in newborns as their liver is still developing.Other
causes of neonatal jaundice include:
- Breast milk jaundice: Occurs in breastfed infants and is caused by a substance in breast milk that inhibits the breakdown of bilirubin.
- Hemolytic jaundice: Caused by the destruction of red blood cells, leading to increased bilirubin production.
- Obstructive jaundice: Occurs when there is a blockage in the bile ducts, preventing the flow of bilirubin from the liver to the intestines.
- Infection or sepsis
- Metabolic disorders
Signs and Symptoms
Jaundice typically presents with a yellow discoloration of the skin and mucous membranes, which is most noticeable in the whites of the eyes. Other signs and symptoms may include:
- Dark yellow urine
- Pale stools
- Lethargy
- Poor feeding
- Weight loss
Assessment and Diagnosis: Newborn With Jaundice Hesi Case Study
Assessment of a newborn with jaundice involves a detailed history and physical examination. The history should include information about the baby’s age, feeding patterns, and any potential risk factors. The physical examination should focus on assessing the extent of jaundice, checking for signs of underlying conditions, and ruling out other causes of yellow discoloration.Diagnostic
tests may be necessary to determine the underlying cause of jaundice. These tests may include:
- Bilirubin levels: Measured in the blood to assess the severity of jaundice.
- Complete blood count: To check for anemia or other hematological abnormalities.
- Liver function tests: To evaluate liver function and identify any underlying liver disease.
- Imaging studies: Such as abdominal ultrasound, to visualize the bile ducts and identify any structural abnormalities.
Differential Diagnosis
The differential diagnosis of neonatal jaundice includes:
- Physiological jaundice
- Breast milk jaundice
- Hemolytic jaundice
- Obstructive jaundice
- Infection or sepsis
- Metabolic disorders
- Gilbert’s syndrome
- Crigler-Najjar syndrome
Treatment and Management

The treatment of neonatal jaundice depends on the underlying cause and severity of jaundice.
Phototherapy, Newborn with jaundice hesi case study
Phototherapy is the most common treatment for neonatal jaundice. It involves exposing the baby to blue or white light, which helps break down bilirubin into a form that can be excreted in the urine.
Exchange Transfusion
In severe cases of jaundice, an exchange transfusion may be necessary. This procedure involves removing the baby’s blood and replacing it with donor blood, which helps lower bilirubin levels.
Other Treatment Options
Other treatment options may include:
- Increased fluid intake: To promote the excretion of bilirubin in the urine.
- Breastfeeding support: To ensure adequate nutrition and hydration.
- Medication: Such as phenobarbital, which can help increase the liver’s ability to metabolize bilirubin.
Nursing Care

Nursing care for newborns with jaundice focuses on monitoring, safety, and education.
Monitoring Parameters
Nurses should monitor the baby’s:
- Vital signs: Temperature, heart rate, respiratory rate, and blood pressure.
- Bilirubin levels: To assess the effectiveness of treatment and prevent kernicterus.
- Feeding patterns: To ensure adequate hydration and nutrition.
- Skin integrity: To prevent skin breakdown under phototherapy lights.
Safety Considerations
Nurses should take precautions to prevent kernicterus, a rare but serious condition that can occur if bilirubin levels become too high. This includes:
- Monitoring bilirubin levels closely.
- Using phototherapy as prescribed.
- Preventing dehydration.
- Avoiding medications that can increase bilirubin levels.
Patient and Family Education
Nurses should educate parents and caregivers about:
- The causes and symptoms of jaundice.
- The treatment options available.
- The importance of monitoring and follow-up care.
- The signs and symptoms of kernicterus.
General Inquiries
What are the common causes of neonatal jaundice?
Physiological jaundice, breast milk jaundice, and hemolytic jaundice are common causes.
How is neonatal jaundice diagnosed?
Diagnosis involves a physical examination, bilirubin levels, and other laboratory tests to determine the underlying cause.
What is the primary treatment for neonatal jaundice?
Phototherapy is the primary treatment, using light to break down bilirubin for excretion.